NHMRC Ideas 2038040, Jan 2025 to Dec 2029
 Aphasia is an acquired language disorder resulting from injury to language areas of the brain, and is a common and debilitating consequence of stroke. Optimal management and treatment of aphasia depends first on carrying out a comprehensive and accurate assessment of the nature and severity of the aphasia. It is essential to determine which language domains are impaired or spared (e.g., word finding, expressive syntax, receptive syntax, etc.) so that interventions can be targeted to the needs of the individual. There are several widely used batteries of tests for aphasia assessment in English and other European languages, but there are presently no validated aphasia batteries in most of the languages of the world. In particular, there are no aphasia batteries in any of the traditional languages or creoles spoken by Aboriginal and Torres Strait Islander peoples. The goal of this project is to create a “universal” aphasia battery and to “instantiate” it in several traditional languages and creoles. For the battery to be “universal” means that its items will not make reference to specific word forms (e.g., “name a stethoscope”) but will instead be defined in terms of linguistic properties (e.g., “name a low-frequency man-made item with a phonologically complex 3-syllable name”). This structure will enable the battery to be instantiated faithfully in any language or dialect, rather than being translated or adapted from a source language. We will develop specific items to create aphasia batteries in Kalaw Kawaw Ya, Yumplatok (Torres Strait Creole), Pintupi-Luritja, Pitjantjatjara, Warlpiri, NT Kriol, Aboriginal English, and standard Australian English. This work will result in validated aphasia batteries ready for clinical use in several widely spoken traditional languages and creoles, as well as a foundation for development of aphasia batteries in other Indigenous languages of Australia and other community languages spoken in Australia and across the world.
Aphasia is an acquired language disorder resulting from injury to language areas of the brain, and is a common and debilitating consequence of stroke. Optimal management and treatment of aphasia depends first on carrying out a comprehensive and accurate assessment of the nature and severity of the aphasia. It is essential to determine which language domains are impaired or spared (e.g., word finding, expressive syntax, receptive syntax, etc.) so that interventions can be targeted to the needs of the individual. There are several widely used batteries of tests for aphasia assessment in English and other European languages, but there are presently no validated aphasia batteries in most of the languages of the world. In particular, there are no aphasia batteries in any of the traditional languages or creoles spoken by Aboriginal and Torres Strait Islander peoples. The goal of this project is to create a “universal” aphasia battery and to “instantiate” it in several traditional languages and creoles. For the battery to be “universal” means that its items will not make reference to specific word forms (e.g., “name a stethoscope”) but will instead be defined in terms of linguistic properties (e.g., “name a low-frequency man-made item with a phonologically complex 3-syllable name”). This structure will enable the battery to be instantiated faithfully in any language or dialect, rather than being translated or adapted from a source language. We will develop specific items to create aphasia batteries in Kalaw Kawaw Ya, Yumplatok (Torres Strait Creole), Pintupi-Luritja, Pitjantjatjara, Warlpiri, NT Kriol, Aboriginal English, and standard Australian English. This work will result in validated aphasia batteries ready for clinical use in several widely spoken traditional languages and creoles, as well as a foundation for development of aphasia batteries in other Indigenous languages of Australia and other community languages spoken in Australia and across the world.
NIH R01 DC013270, Jun 2020 to May 2025
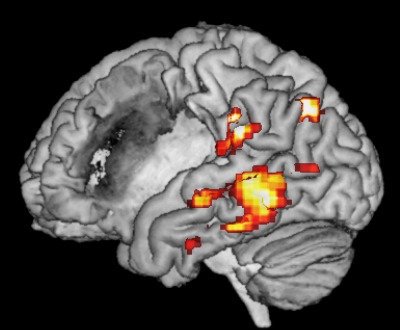 Aphasia is one of the most common and debilitating consequences of stroke. Aphasia is caused by damage to language regions of the brain, which are usually localized to the left hemisphere. Fortunately, most individuals with aphasia after a stroke experience some degree of recovery of language function over time. The pace of recovery is greatest in the first weeks and months, but clinically meaningful gains in language function are possible even years after stroke. Recovery from aphasia is thought to depend on neural plasticity, that is, functional reorganization of surviving brain regions such that they take on new or expanded roles in language processing. However, despite much research, the mechanisms that underlie this process of functional reorganization remain poorly understood. The overall goals of this project are to better characterize the neural correlates of recovery from aphasia after stroke, and to determine which patterns of functional reorganization are associated with more or less favorable language outcomes.
Aphasia is one of the most common and debilitating consequences of stroke. Aphasia is caused by damage to language regions of the brain, which are usually localized to the left hemisphere. Fortunately, most individuals with aphasia after a stroke experience some degree of recovery of language function over time. The pace of recovery is greatest in the first weeks and months, but clinically meaningful gains in language function are possible even years after stroke. Recovery from aphasia is thought to depend on neural plasticity, that is, functional reorganization of surviving brain regions such that they take on new or expanded roles in language processing. However, despite much research, the mechanisms that underlie this process of functional reorganization remain poorly understood. The overall goals of this project are to better characterize the neural correlates of recovery from aphasia after stroke, and to determine which patterns of functional reorganization are associated with more or less favorable language outcomes.
NIH R01 DC013270, Jun 2014 to May 2020
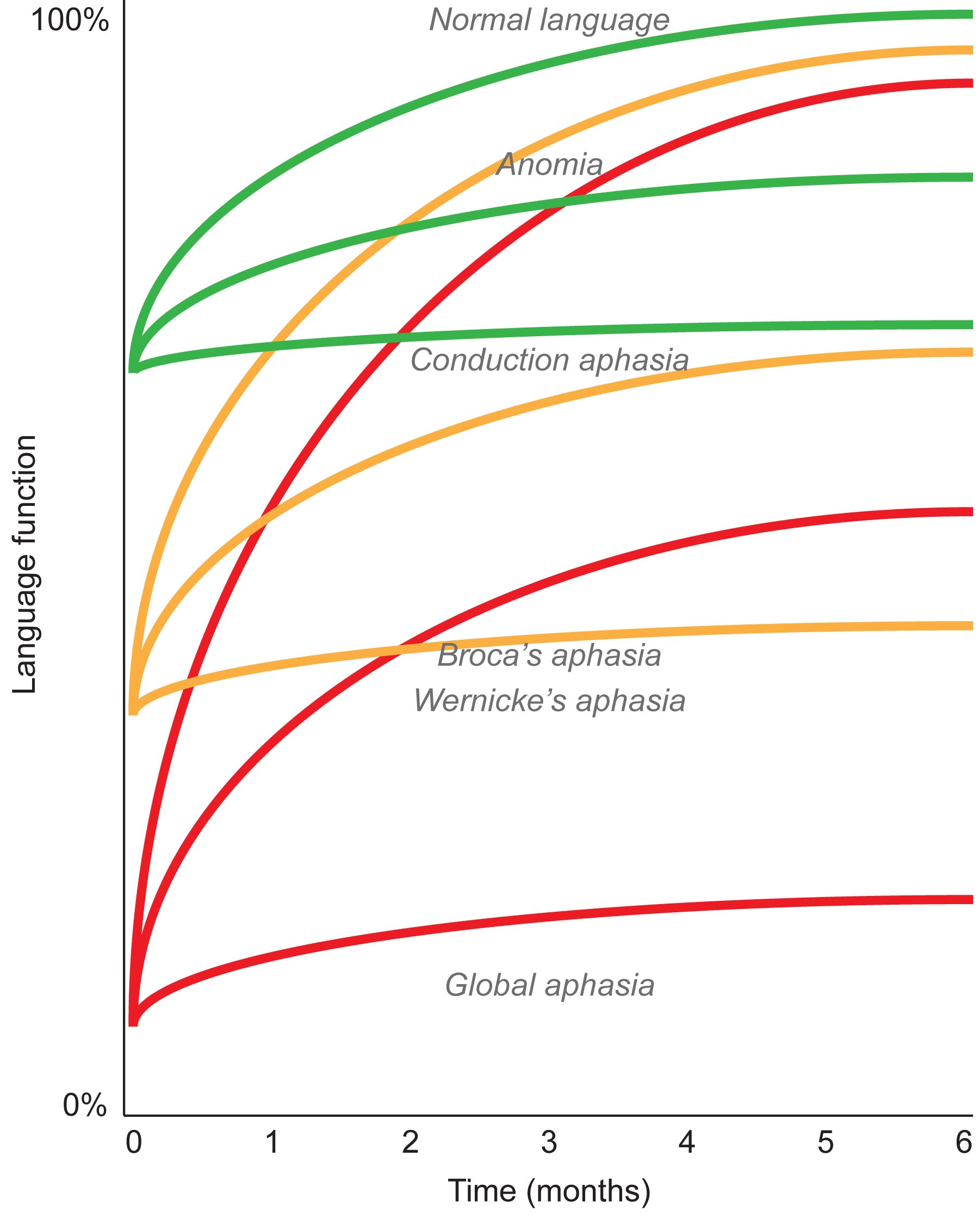 The overall goal of this project is to identify the neural correlates of recovery from aphasia during the first three months after acute stroke. Aphasia is one of the most common and debilitating consequences of strokes affecting the dominant hemisphere. In the acute and subacute stages, most patients experience some degree of recovery of language function. These first few months after brain damage occurs are critically important because the greatest behavioral gains take place during this time, even when patients do not receive treatment. However the extent of recovery is highly variable: some patients recover most or nearly all language function, while others make few gains and remain chronically aphasic. It is not well understood what neural mechanisms underlie recovery during this period, nor why some patients recover so much better than others. To address these questions, we propose to study individuals with aphasia due to acute left hemisphere stroke. A better understanding of the neural correlates of successful recovery will improve the accuracy of prognoses so as to better plan medical treatments and behavioral interventions.
The overall goal of this project is to identify the neural correlates of recovery from aphasia during the first three months after acute stroke. Aphasia is one of the most common and debilitating consequences of strokes affecting the dominant hemisphere. In the acute and subacute stages, most patients experience some degree of recovery of language function. These first few months after brain damage occurs are critically important because the greatest behavioral gains take place during this time, even when patients do not receive treatment. However the extent of recovery is highly variable: some patients recover most or nearly all language function, while others make few gains and remain chronically aphasic. It is not well understood what neural mechanisms underlie recovery during this period, nor why some patients recover so much better than others. To address these questions, we propose to study individuals with aphasia due to acute left hemisphere stroke. A better understanding of the neural correlates of successful recovery will improve the accuracy of prognoses so as to better plan medical treatments and behavioral interventions.
NIH R21 DC016080, Apr 2017 to Mar 2020
In many individuals with acquired aphasia, language function improves to some extent over time. This recovery process is thought to depend on neuroplasticity, that is, functional reorganization of brain regions involved in language processing. There is great interest in characterizing this reorganization process, and determining whether it can be facilitated by behavioral, neuromodulatory or pharmacological interventions. However, a major roadblock to this line of research is that it is challenging to identify language regions of the brain in individuals with aphasia. Tasks commonly used to engage language processing, such as narrative comprehension and picture naming, are limited in terms of validity (identification of language regions, and not other regions) and reliability (test-retest reproducibility). On the other hand, paradigms such as semantic decision that are effective in mapping language in people without aphasia (for instance, presurgical patients), are typically too challenging for people with aphasia. The overall goal of this study is to develop an adaptive semantic matching paradigm that can be successfully performed by people with aphasia, and that is valid and reliable in identifying language regions in individual patients. The key innovation is an adaptive staircase procedure whereby each individual is presented with stimuli that are challenging yet within their competence, so that language processing can be fully engaged in people with and without language disorders. The feasibility, validity and reliability of this adaptive semantic matching paradigm will be evaluated and compared to two commonly used paradigms: narrative comprehension and picture naming. It is hypothesized that the adaptive semantic matching paradigm will be more effective than these commonly used paradigms. The experimental control scripts, stimuli, and normative brain imaging data will be made freely available to other researchers. Moreover, this study will establish a formal framework for quantifying feasibility, validity and reliability of language mapping paradigms in this clinical research context, so that other potential approaches can be similarly evaluated.
NIH R03 DC010878, Jul 2010 to Mar 2014
Primary progressive aphasia (PPA) is a clinical syndrome in which degeneration of language regions in the dominant hemisphere is associated with progressive deficits in speech and/or language function. The overall goals of this project are to use functional magnetic resonance imaging (fMRI) to investigate neural changes underlying linguistic deficits in PPA, and to use this information to better discriminate patients with variants of PPA from each other and from normal aging. Recent studies have identified three clinical variants of PPA: progressive non-fluent aphasia (PNFA), semantic dementia (SD) and logopenic progressive aphasia (LPA). Each variant is associated with characteristic linguistic features, distinct patterns of brain atrophy, and different likelihoods of particular underlying pathogenic processes, making correct differential diagnosis highly relevant. We will recruit 48 patients with PPA (16 of each variant) and 24 normal controls over a three year period, and acquire fMRI data along with structural MRI, linguistic and cognitive measures. The fMRI paradigm consists of a syntactic processing task with seven conditions parametrically varying in syntactic complexity. The research will address two specific aims. The first is to identify the relationships between volume loss, changes in functional MRI activation, and linguistic deficits, in the different PPA variants. The second aim is to improve differential diagnosis of PPA variants using machine learning algorithms incorporating both structural and functional imaging measures.